In our previous blog post in this series on fetal heartrate monitoring, I outlined how the fetal heartrate develops, and how it is monitored at key points during a pregnancy - particularly during active labour. In this post, I'll explain why normal heartrate variability is reassuring to medical providers, what abnormal variability can mean, and what you can do if a loved one has suffered a preventable birth injury from negligent or incompetent obstetrical care.
Written by Roger Shoreman, Senior Law Clerk
Variability and Abnormalities
Obstetricians and midwives look at the variability of the fetal heartrate for an indication of potential fetal distress during active labour. Heartrate variation of between 6-25 bpms is considered "moderate" or normal, as are accelerations of the heartrate during labour (especially in the late stages). If there is minimal variation (less than 5 bpm variation for 40-80 minutes) it's considered atypical and guidelines suggest further monitoring. If minimal variation lasts for more than 80 minutes, if there is marked variation (more than 25 bpm variation for 10 minutes or more), if a sinusoidal pattern is recognized, or if the baseline heartrate is erratic, practitioners will consider these readings abnormal and a sign of fetal distress. Moreover, decelerations (especially repetitive decelerations with complicated variables, late decelerations, or a single prolonged deceleration) are also signs of abnormalities. In addition to sustained irregular variations, abnormally high or low heartrates are cause for serious concern. During a pregnancy, these extremes can point to maternal or in utero infection, maternal health concerns (hyperthyroidism, medication side effects), or dangerous conditions such as placental insufficiency.Fetal Tachycardia and Bradycardia
During active labour, fetal tachycardia (a baseline heartrate over 160 bpm for more than 80 minutes) can signal life-threatening conditions such as fetal hypoxia (absence of oxygen). Severe bradycardia (less than 100 bpm) can point to severe hypoxia due to prolonged cord compression or prolapse, maternal seizures, or rapid fetal descent. If an attending medical practitioner does not adequately monitor these abnormalities, fails to identify them, or does not take appropriate and timely actions to treat the condition or hasten delivery, a baby may sustain significant brain damage from asphyxia (oxygen deprivation). Interventions that are indicated may include a caesarian, vacuum or forceps delivery. Failure to intervene may cause injury and give rise to a negligence action.When Fetal Distress Leads to Permanent Damage
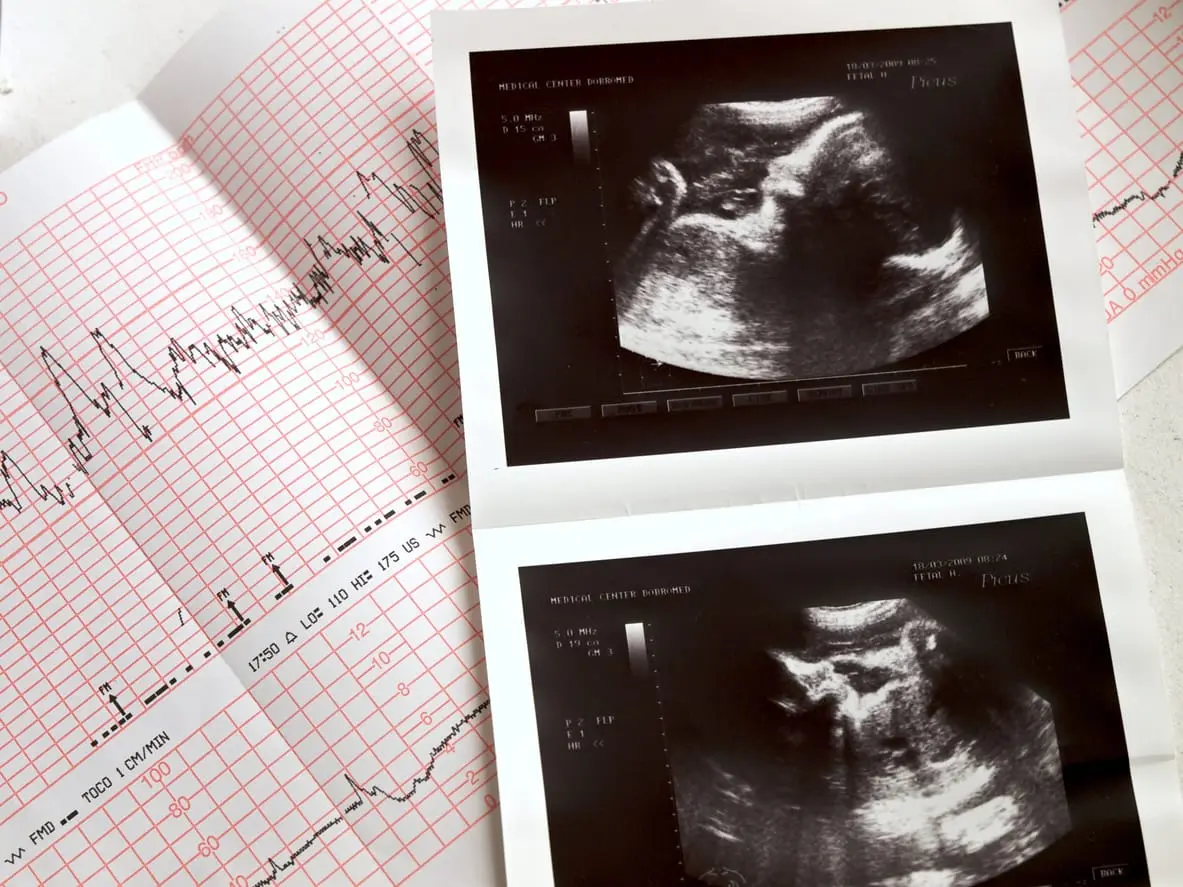
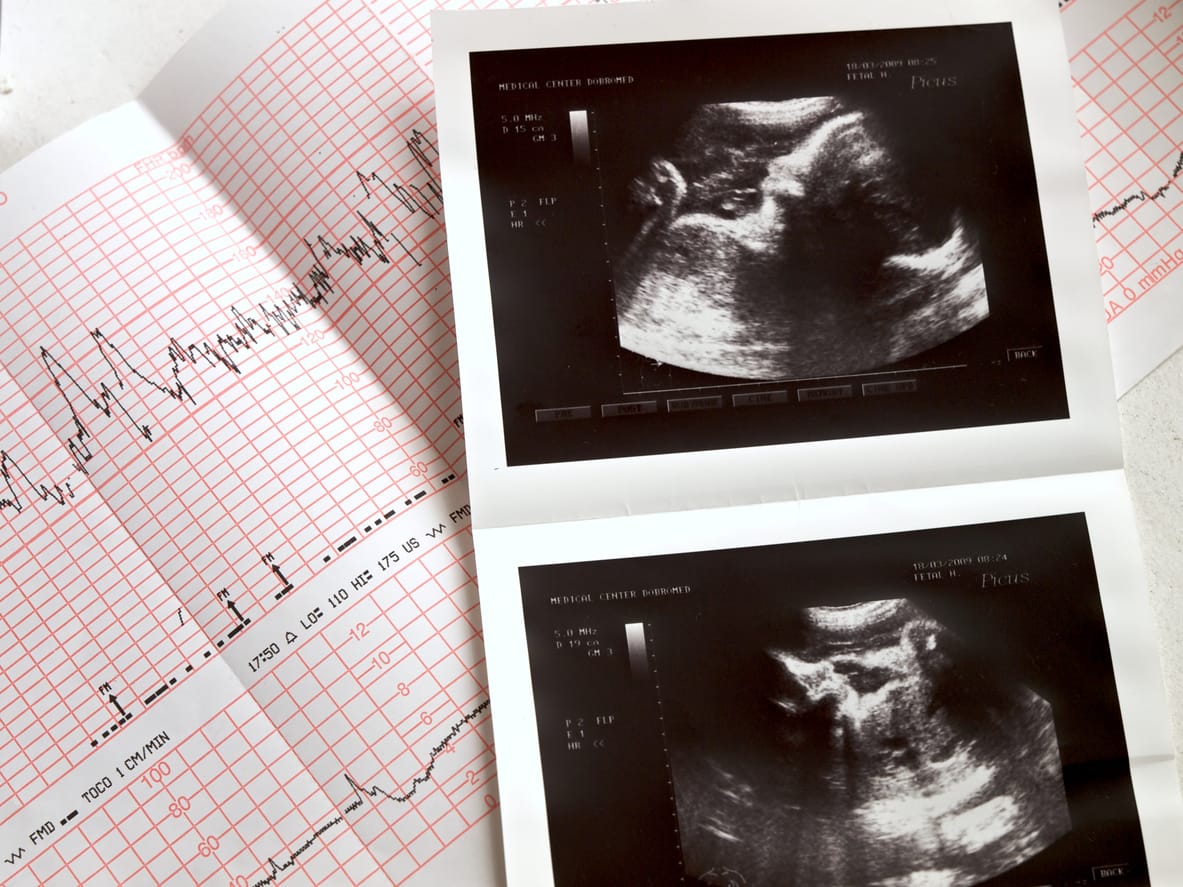
Although some effects of neurological damage will not be immediately apparent, low APGAR scores, abnormal blood-gas measurements and seizures within 12-24 hours tend indicate an asphyxic injury that can be confirmed by an MRI. Neurological damage from fetal distress and asphyxia may cause conditions such as Cerebral Palsy or severe mental and emotional impairment. In a matter of minutes, a newborn may sustain a birth injury that robs them of the opportunity to ever live independently. When a medical practitioner is negligent or incompetent in monitoring the fetal heartrate and it leads to a preventable a birth injury, you can take legal action. As one of the country's top personal injury firms, Gluckstein Lawyers understands what it takes to put together a strong case when making a claim of obstetrical malpractice. Using Auscultation charts, electronic fetal heartrate printouts and other health records in combination with professional guidelines and standards of practice, we can show that critical protocols were not followed and caused serious harm. With our firm's commitment to full-circle care, we are not only able to be your advocate you through the legal process, but also take a keen interest in learning how we can support you and your loved ones as you build a new life when the case concludes. To learn more about how our firm can help, contact us at [email protected].Did you miss Part 1 of this blog series?
You can read part one here.
Comments We would love to hear from you. Please share your thoughts about insurance benefits in "Leave a Comment" found below.
Expertise.
Share
Subscribe to our Newsletter